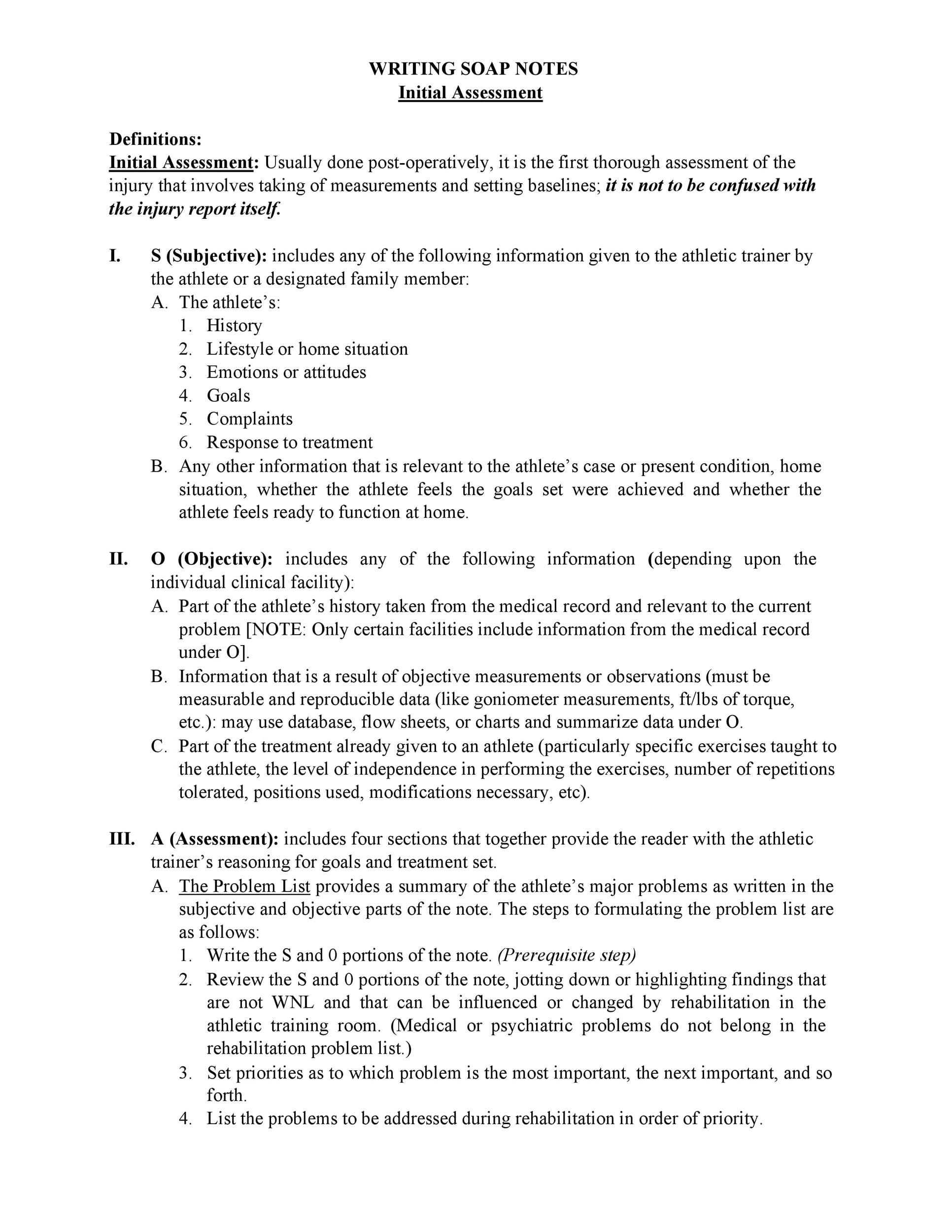
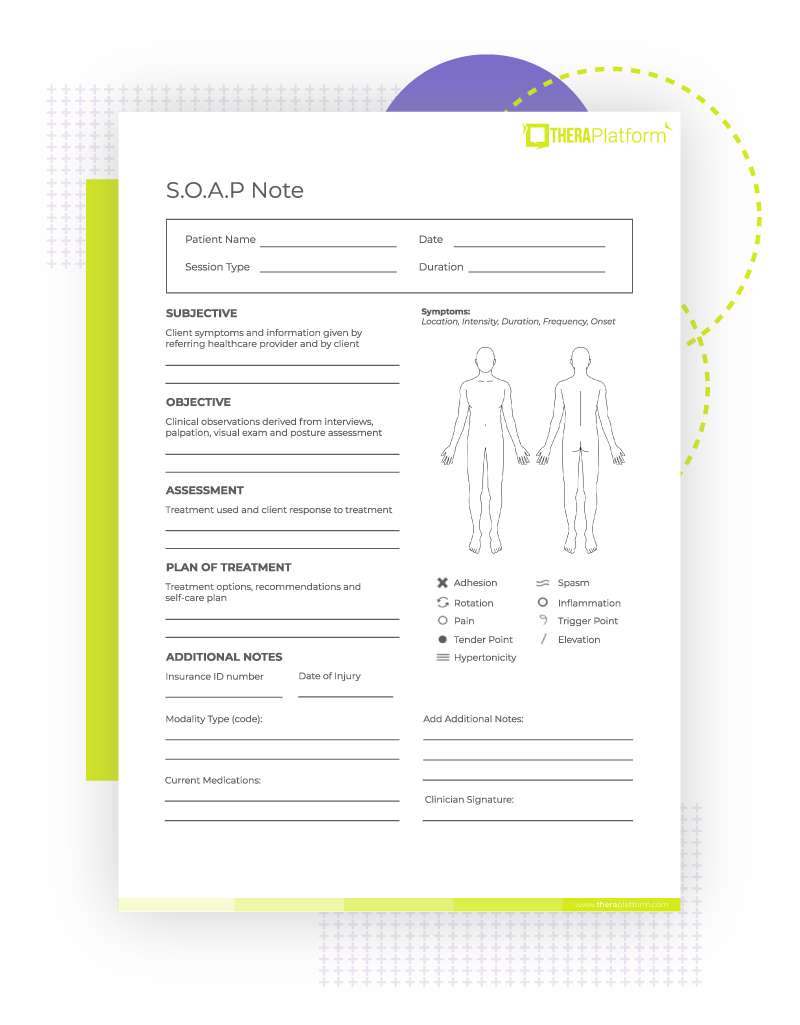
Physical Exam Template Soap Note - Soap notes should include 4 sections—subjective (patient’s symptoms and. A comprehensive soap (subjective, objective, assessment, plan) note detailing the.
Soap notes should include 4 sections—subjective (patient’s symptoms and. A comprehensive soap (subjective, objective, assessment, plan) note detailing the.
Soap notes should include 4 sections—subjective (patient’s symptoms and. A comprehensive soap (subjective, objective, assessment, plan) note detailing the.
Soap Note Template 33 Medical Diagnosis Physical Examination
A comprehensive soap (subjective, objective, assessment, plan) note detailing the. Soap notes should include 4 sections—subjective (patient’s symptoms and.
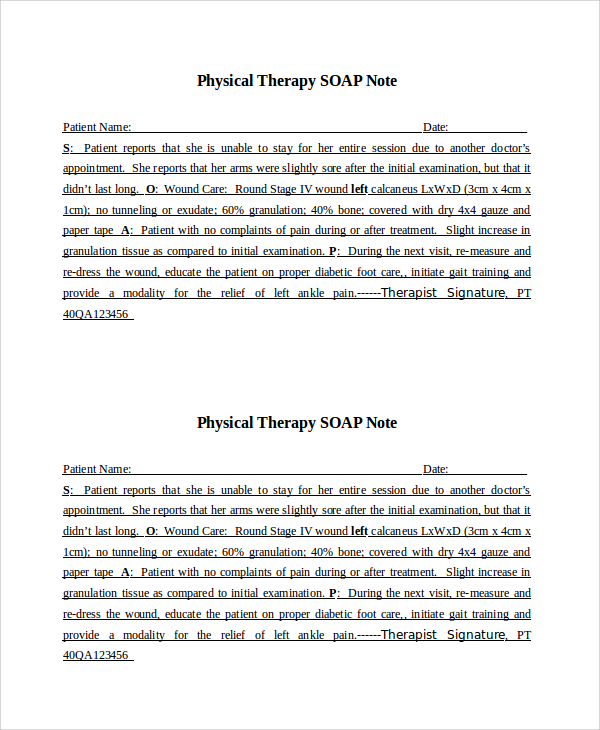
SOAP Notes For Physical Therapy Template & Example Free PDF Download
Soap notes should include 4 sections—subjective (patient’s symptoms and. A comprehensive soap (subjective, objective, assessment, plan) note detailing the.
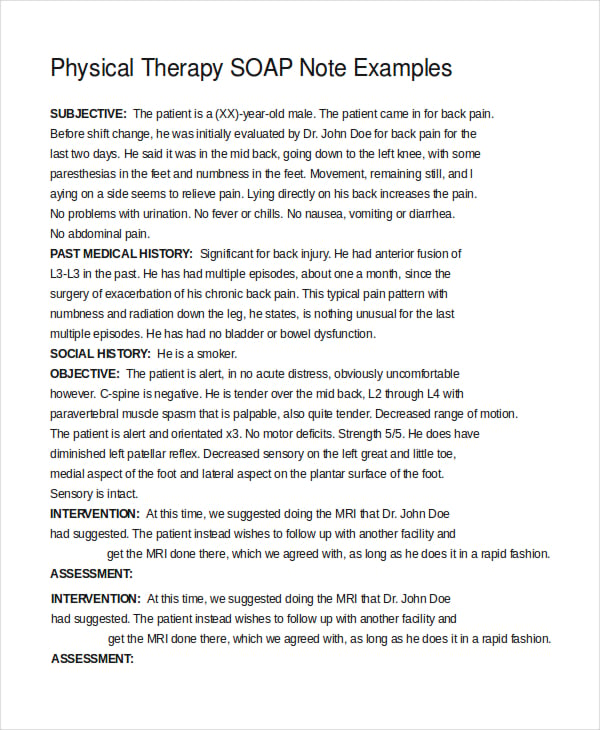
FREE 15+ SOAP Note Templates in PDF MS Word
A comprehensive soap (subjective, objective, assessment, plan) note detailing the. Soap notes should include 4 sections—subjective (patient’s symptoms and.
Soap Note Physical Therapy Sample
A comprehensive soap (subjective, objective, assessment, plan) note detailing the. Soap notes should include 4 sections—subjective (patient’s symptoms and.
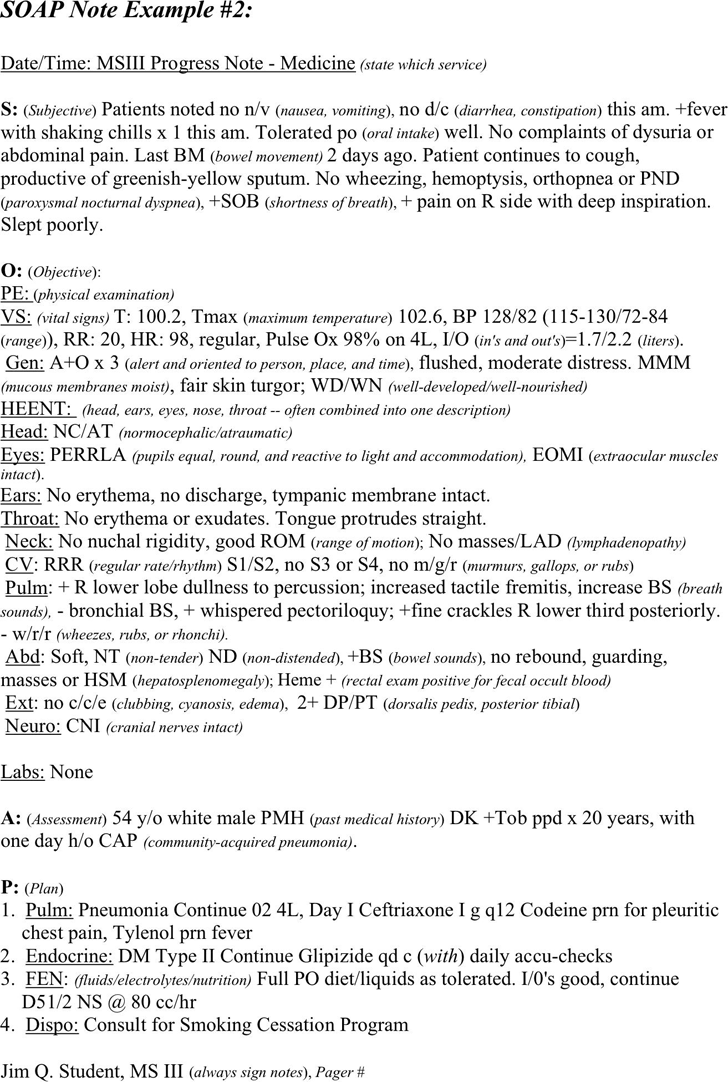
Free SOAP Note Example PDF 102KB 1 Page(s)
A comprehensive soap (subjective, objective, assessment, plan) note detailing the. Soap notes should include 4 sections—subjective (patient’s symptoms and.
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab
A comprehensive soap (subjective, objective, assessment, plan) note detailing the. Soap notes should include 4 sections—subjective (patient’s symptoms and.
Physical Therapy SOAP Note Interactive PDF Template
Soap notes should include 4 sections—subjective (patient’s symptoms and. A comprehensive soap (subjective, objective, assessment, plan) note detailing the.
Free SOAP Notes Template ClinicSense
A comprehensive soap (subjective, objective, assessment, plan) note detailing the. Soap notes should include 4 sections—subjective (patient’s symptoms and.
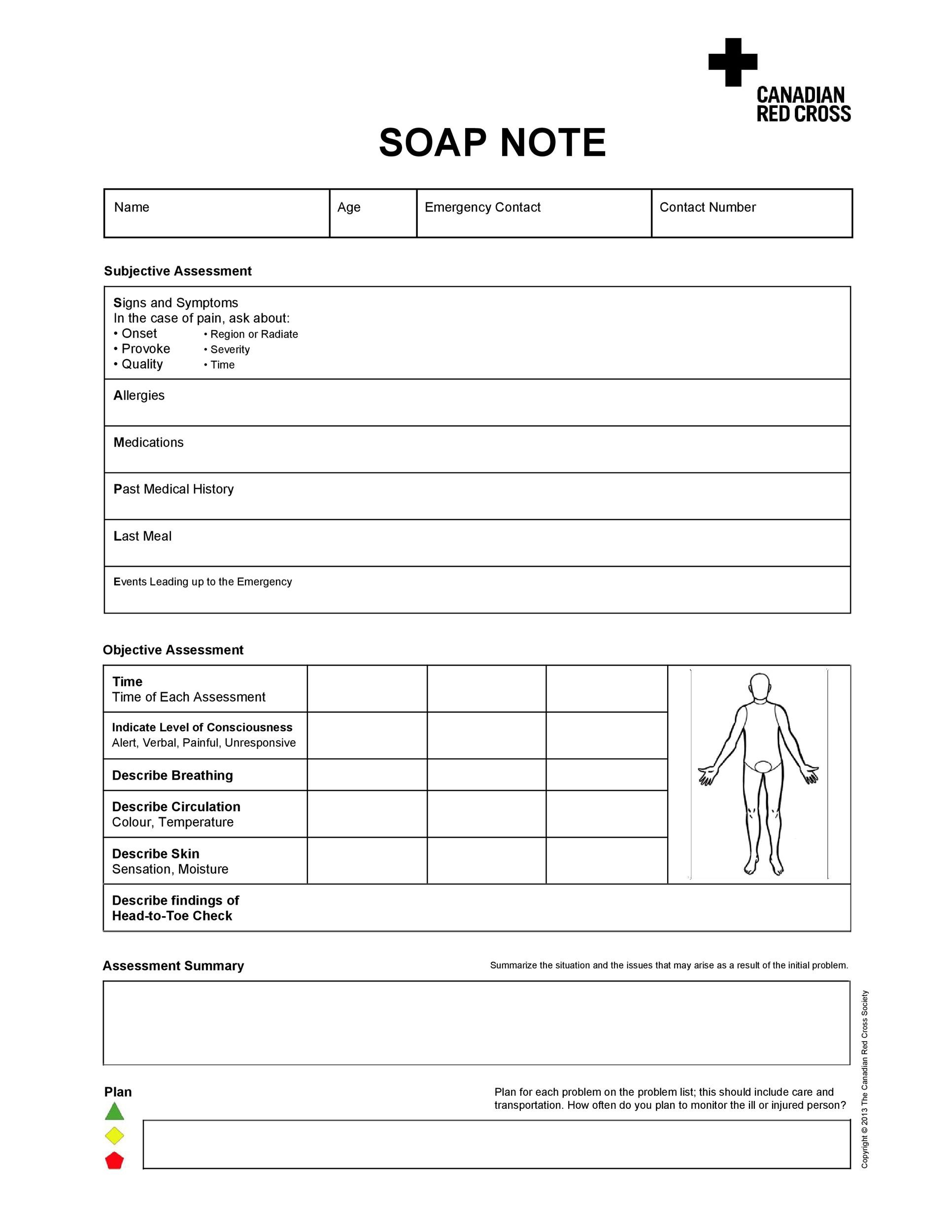
Physical Exam Template Soap Note
Soap notes should include 4 sections—subjective (patient’s symptoms and. A comprehensive soap (subjective, objective, assessment, plan) note detailing the.
A Comprehensive Soap (Subjective, Objective, Assessment, Plan) Note Detailing The.
Soap notes should include 4 sections—subjective (patient’s symptoms and.

.png)